New GLP-1 Guidelines Just Dropped - The Who, What, Where, When, Why and How of Weight Loss Drug Management
GLP-1 medications like Ozempic and Wegovy are on the rise, with 12% of U.S. adults having tried them. But new medical guidelines make one thing clear: these meds aren't enough on their own.

Welcome to the GLP-1 era—a moment that’s been 20 years in the making. While the FDA first approved GLP-1s in 2005, 6% of Americans are now on medications like Ozempic, Wegovy, Mounjaro, and Zepbound, and 12% of US adults have tried a GLP-1—and that number keeps climbing.
However, I’ve noticed that the guidance around GLP-1s can often feel pretty reductive: Eat less. Take your weekly shot. Lose weight. But that’s far from the full picture.
On May 30, four major medical organizations published new guidelines on how to support people on GLP-1s, and they made one thing very clear: GLP-1s alone aren’t enough.
The Full GLP-1 Picture
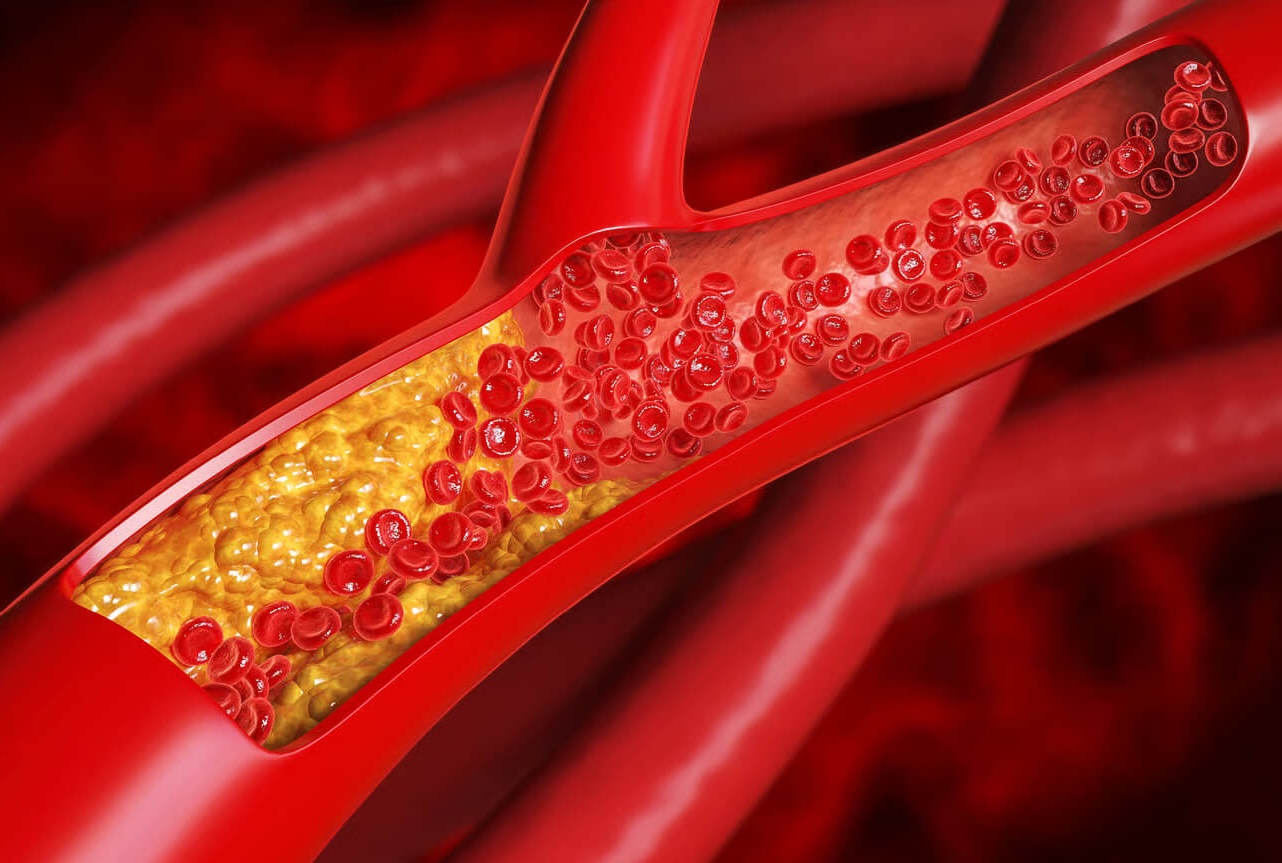
GLP-1s drive 5-18% weight loss in clinical trials, but they’re not without trade-offs. Potential side effects include nausea and vomiting, nutrient deficiencies, and muscle and bone loss.
This is why doctors can’t simply prescribe a GLP-1 and send a patient off on autopilot. Patients need comprehensive support and follow-up, and that’s exactly what these new guidelines emphasize.

Their research found that patients who pair GLP-1 therapy with structured nutrition and behavioral support are more likely to be consistent with treatment, lose more weight, and actually maintain that weight loss after stopping medication.
Sounds great! But what does this care look like? Let’s start with nutrition:
Protein: The Biggest Part of The GLP-1 Puzzle
Here’s something most people don’t realize: When you lose weight, you’re losing a mix of fat and muscle. And for people taking GLP-1s, that muscle loss tends to be more pronounced.
This is important because lean body mass is critical for long-term health, strength, metabolism, and aging well. So we need to be smart about how to minimize this risk.
The good news is you can mitigate it by lifting weights at least three times per week and eating enough protein. The bad news is that we still haven’t reached a consensus on how much protein is “enough” (you’d think we’d have solved this by 2025).
- Here’s Why: The National Academy of Medicine's long-standing recommendation of 0.8 grams per kilogram of body weight was created to prevent disease rather than to optimize good health.
So what should you aim for? Most clinicians now recommend 80-120 grams of protein per day, or about 16–24% of your total calories on a 2,000-calorie diet.
But if I were your doctor? I’d recommend you divide your current body weight by 2.2, then multiply it by 1.6. That number gives you a solid target range to account for fluctuating calorie intake (which is super common on GLP-1s).

Muscle Mass vs. Muscle Weight
We’ve covered preventing muscle loss. But the guidelines bring up another important piece of the puzzle—muscle health. There’s a big difference, because you can maintain muscle mass on paper but still get weaker and lose the ability to do everyday activities.

Beyond Food and Exercise
Here's where these guidelines get interesting—they emphasize that your physical health is deeply connected to everything else in life. That means paying attention to:
- Sleep Quality: Poor sleep messes with the hormones that control hunger, which can work against your GLP-1 medication. Aim for 7-9 hours of sleep every night.
- Alcohol Intake: Not only will it mess with your sleep quality, but excessive drinking can increase the risk of GLP-1 side effects.
- Stress Management: Chronic stress induces cortisol, which can increase cravings for high-calorie foods. Find ways to mitigate stress through yoga, therapy, meditation, or walks (without your phone).
- Social Support: This is where behavioral support comes in. Having people who understand your health journey makes you more likely to stick with it. Try to find accountability partners or support groups.
This Takes Time, Attention, and Partnership
The final message of these new guidelines is one I emphasize with Ajenda members, friends, and past patients every day: GLP-1 medications aren’t a magic bullet—they’re a tool. And like any tool, their effectiveness depends on how we use them.
That means adding nutritional monitoring, regular check-ins, and individualized adjustments as part of your treatment plan. Because the women who see the best long-term results?
They treat their GLP-1 medication as one piece of a comprehensive health strategy, not the entire strategy itself.