Fitness Guides
I Thought It Was Impossible to Increase Bone Mineral Density After 50. I Was Wrong.
For years, I believed the best we could do after menopause was slow bone loss — until a repeat DEXA scan showed my bone mineral density actually increased. Here’s what the science says about building bone after menopause, and what worked for me.

For almost 20 years, I’ve told people some version of this: “After menopause, the best we can usually do is slow the loss of bone density.”
In many cases, that’s true. But I just learned that it’s also incomplete.
I recently had a DEXA Scan (a test that measures bone strength) on the exact same machine as my scan from one year ago. The result? My bone mineral density (BMD) increased by 2.4%. (By the way, the recommendation for a woman with normal BMD is to repeat a DEXA in 2 or more years, not 1 year as I did.)
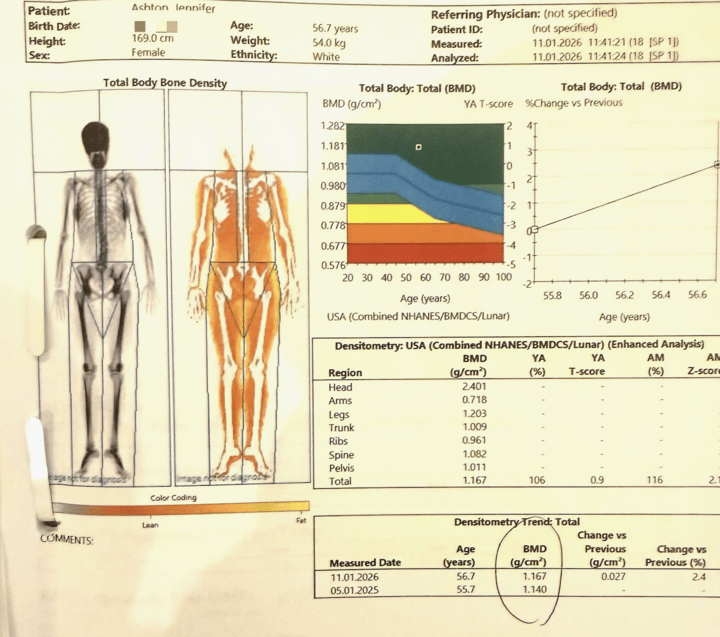
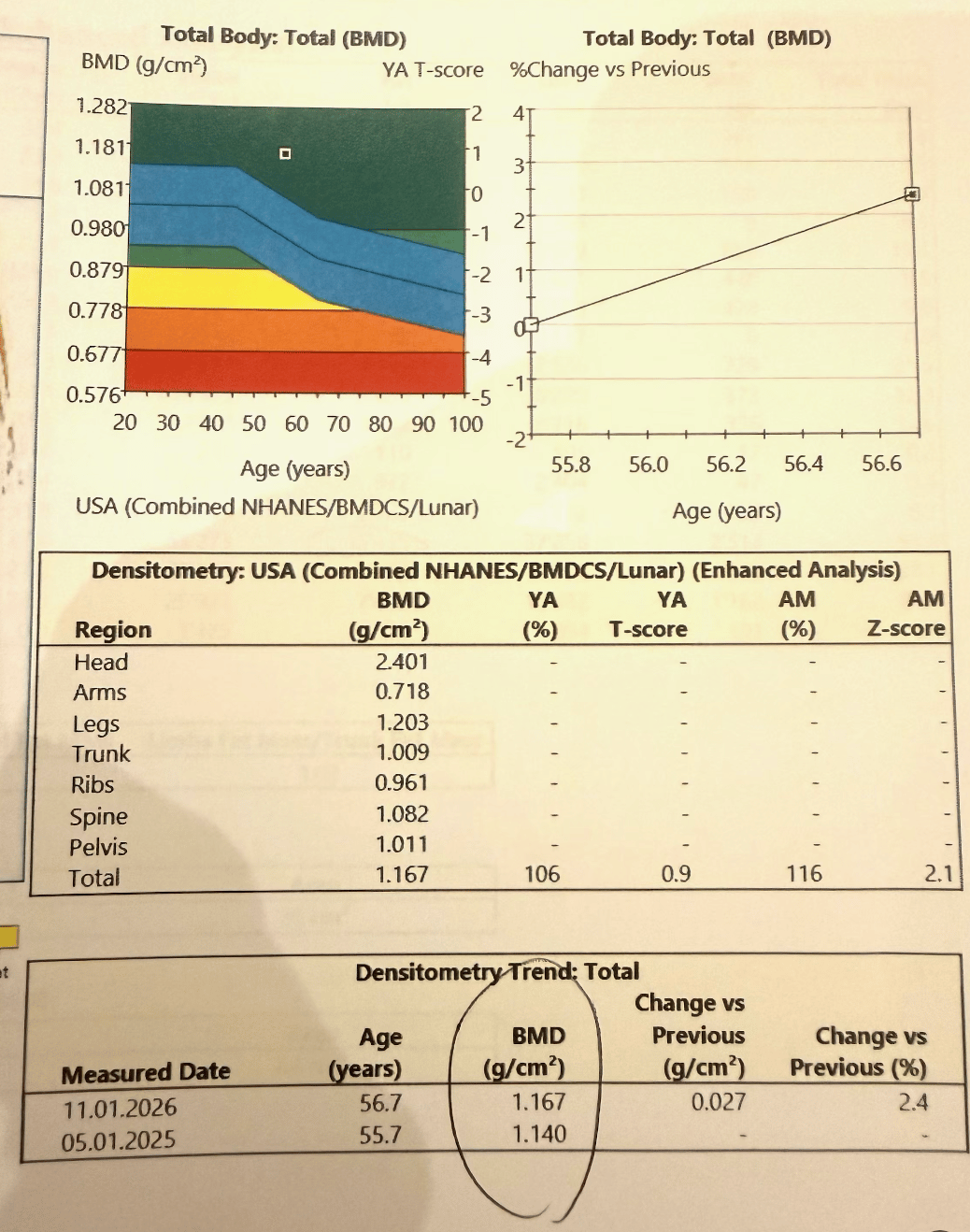
This wasn’t a rounding error or a fluke. It was the same equipment. The result was so clear it forced me to say out loud: Jen, I cannot believe my eyes. Sit down. Your skeleton has notes.
Building Bone After Menopause
What happened here? Let me walk you through what the research says and then what I believe made the difference for me.
First, a reality check. Increasing BMD after 50 is hard. It requires consistent effort and the right interventions. But it’s not some mythical outcome. Research shows two main things move the needle:
- Hormone Therapy (HRT): In peer-reviewed trials, menopausal hormone therapy has been shown to preserve and increase BMD and reduce fracture risk compared with placebo.
- Heavy Lifting: Resistance training (lifting heavier weights over time) shows measurable benefit for BMD in postmenopausal women.
The punchline from more recent reviews is what many of us see clinically: the combination of an estrogen-supportive hormonal environment plus structured loading is generally more effective than either alone.
That said? Here are the details on what I’ve done that likely contributed to increasing my bone mineral density:
1) HRT (five years and counting).
I’ve been on HRT for five years. Estrogen has a documented role in bone remodeling, and randomized trials have shown BMD benefits with hormone therapy.
2) Heavy resistance training.
Not “cute little 3-pound weights.” I’m talking progressive overload: lifting heavy enough that my body has to adapt.
If you follow me on Instagram, you know that for the past 18 months I’ve been doing exactly that with professional trainer Korey Rowe. It’s why I’m stronger today at 56 than I was at 36. And my scan shows that his training approach, and my Wellness Experiment pays dividends in truly significant ways.
This isn’t just anecdotal. Research shows that resistance training is a powerful lever for increasing BMD in postmenopausal women.
It is true that my bones were good before I started training with Korey. In fact, my bone mineral density was in the normal range (not even osteopenia) because I’ve been lifting weights since high school.
This is your reminder that the window of adolescence and early 20’s is key for preventing osteopenia or osteoporosis 30-40 years later! So if you know a teenage girl or young woman in her 20’s, pay it forward and share this key bone-sparing info with her!
3) Getting ~1,200 mg/day of calcium from food.
I’ve been militant about getting 1,200 mg of calcium from food (not supplements) every day. The data is clear: calcium in supplement form is not a reliable fracture-prevention strategy for most postmenopausal women.
- Science Says: A 2015 review found that the evidence that calcium supplements prevent fractures is “weak and inconsistent.”
That doesn’t mean calcium doesn’t matter. It means how you get it matters, and food-first is usually the cleanest approach.
Vitamin D3 and Vitamin K2 are part of this, too. Vitamin D is essential for calcium absorption and bone metabolism. Vitamin K2 (menaquinone) has suggested benefitsfor lumbar spine BMD and fracture outcomes in postmenopausal women.
The One Thing I Want You To Hear
Do not wait until you’re 65 to start thinking about your bones.
While the USPSTF recommends routine osteoporosis screening with DXA starting at age 65 for most women, I have never followed these recommendations.
Why? Because I was trained to get a baseline DEXA when menopause starts. And in my medical career, I’ve seen numerous cases of osteoporosis in women aged 50. I subscribe to the philosophy of: I would rather catch something sooner rather than later, and since we ALL lose bone density as we age, I would rather know about it at 50 rather than 65!
I encourage you to be aggressive about asking your health care provider or doctor about getting a DEXA scan when you go through menopause or at least before age 65.
The good news? Your skeleton is a living tissue that can respond to the right inputs. This experience reminded me of exactly why I love medicine and being a physician: the body can do miraculous things!


