Nutrition Advice
Low Bone Density and Algae-Derived Calcium: What Does The Science Show?
Algae-derived calcium is being marketed as a safer, more “natural” way to support bone health—but when you look past the green halo, the science tells a more cautious story.
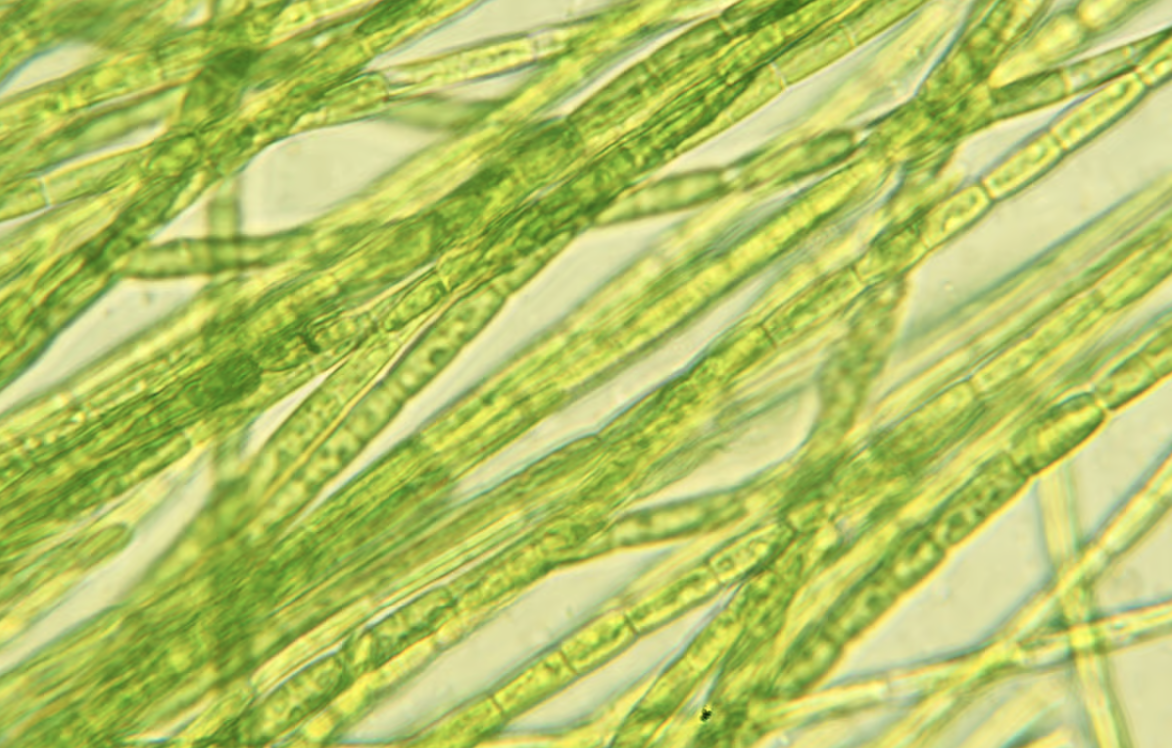
Algae-derived calcium is having a major moment. It’s being marketed as the “gentler,” more “natural” alternative to traditional calcium supplements, with claims that it’s easier on the stomach and more “body-friendly.”
It sounds perfect. But as a doctor, I’ve learned to look past the “plant-based” halo. We need to ask ourselves: Does it actually improve bone mineral density (BMD)? And can it lead to fewer fractures without the downsides we worry about with supplemental calcium?
Let’s see for ourselves:
Quick Recap: The Risks of Supplemental Calcium
Calcium supplements are controversial for two reasons:
- Kidney Stones: Large-scale studies, like the Women’s Health Initiative (WHI), found that calcium and vitamin D supplements increased the risk of urinary tract stones by 17%.
- Cardiovascular Risk: The evidence is a bit of a mixed bag, but there is definitely some data that suggests a link between calcium supplements and an increased risk of heart attacks. This is NOT new, and it is why the doctors who have been current with medical literature have advised AGAINST most women taking calcium in supplemental form after menopause. Not only does the data show it doesn’t HELP reduce the risk of osteoporotic fractures, but the data DOES suggest it HARMS cardiovascular and renal health.
Let’s be clear: algae calcium is still supplemental calcium. It doesn’t sidestep the risks of kidney stones and heart health just because it’s “green.” Until we have safety data, the same caution applies.
Now that we’ve cleared that up, let’s tackle the claim that algae-based calcium improves bone mineral density, which translates to fracture prevention.
BMD is Not The Same as Fracture Prevention
A DEXA scan (dual-energy X-ray absorptiometry) measures how strong your bones are. While a higher score of bone mineral density is a good thing, it’s not a guarantee that you’re safe from fractures.
The truth is, you can have “dense” bones on paper and still break a hip if you have poor balance, blurry vision, weak muscles, or are on certain medications.
This is why small improvements in a bone scan don't always translate into a real-world fracture reduction. Ultimately, a “BMD claim” on a supplement bottle is not a promise of “fracture prevention.”
Do We Have Any Clinical Trials on Algae-Derived Calcium?
The most rigorous data we have comes from a 24-month study on postmenopausal women using Aquamin (a common algae-calcium brand) with or without a prebiotic. The research found:
- No significant improvement in bone mineral density after two years in either the calcium-only or calcium and prebiotic groups compared to placebo.
- However, both calcium groups appeared to slow bone turnover, which theoretically could be protective, but didn’t translate to measurable bone mineral density gains.
That distinction matters. As we get older, a good goal for us to have is slowing the rate of bone loss, rather than hoping for a single supplement that will “grow bone.”
But let’s be crystal clear: there is a long leap between “favorably affecting markers of bone turnover” and “slowing bone loss” to “building new bone” and ultimately “reducing the risk of osteoporotic fractures.” People use them interchangeably, but they are NOT the same thing, and so we have to be cautious with concluding one with the other.
The Honest Framing of Algae-Derived Calcium
When we strip away the marketing, the honest way to frame algae-derived calcium is this:
- Best Case: Based on current data, it may help maintain bone mineral density, slow loss, and improve turnover markers in postmenopausal women.
- Unknown: It’s still too far of a leap to say it reduces your risk of osteoporotic fractures, nor do we have proof that it sidesteps the kidney and heart risks associated with traditional supplemental calcium.
What This Means For You
If you were my patient, here’s what I’d tell you:
- Start with your plate. Get your calcium from food (dairy, fortified soy, canned salmon/sardines with bones, calcium-set tofu, leafy greens). These foods come with protein and micronutrients that support bone and muscle.
- Don’t guess, assess. If you absolutely cannot reach your needs with food (which is possible), talk to your doctor about smaller supplemental doses at ≤500–600 mg per dose. While you’re at it, check your Vitamin D levels. Remember, more is not better. The theory about why supplemental calcium may be harmful for most women is that it causes an abrupt increase in blood calcium levels, so truly, more is really not better.
- Focus on the heavy hitters. If you’re osteopenic or osteoporotic, the real protection comes from resistance training, adequate protein, and FDA-approved osteoporosis medications when indicated. These all have stronger outcome data for fracture risk than any single calcium form.
Bottom line: algae-derived calcium is an interesting option with some supportive human data for maintenance of BMD, but the leap from “BMD support” to “fracture prevention” is far-fetched. Not to mention, the safety around calcium supplements still applies.


